The Gut-Immune Connection: How Your Digestive Health Affects Immunity
Introduction
In recent years, the connection between gut health and the immune system has garnered significant attention in both scientific research and popular health discourse. The gut, often dubbed "the second brain," plays a crucial role not only in digestion but also in maintaining overall health, particularly in immune function. In this article, we will delve into how the health of your digestive system can directly influence your immune response and what you can do to enhance both.
Understanding the Gut-Immune Connection
The Anatomy of the Gut
The gastrointestinal (GI) tract extends from the mouth to the anus and is home to trillions of microorganisms collectively referred to as the gut microbiome. This intricate community comprises bacteria, viruses, fungi, and other microbes that digest food, synthesize vitamins, and protect against harmful pathogens.
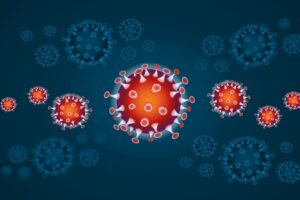
The Immune System Overview
The immune system is the body’s defense mechanism against disease-causing pathogens like bacteria, viruses, and parasites. It comprises various cell types (like T cells and B cells), tissues, and organs, including the spleen, thymus, and lymph nodes. A significant portion of the immune system (about 70%) is located in the gut-associated lymphoid tissue (GALT).
The Gut-Immune Axis
The gut-immune axis refers to the bidirectional relationship between the gut microbiome and the immune system. The gut microbiome influences the development and function of immune cells, while the immune system affects the composition of the gut microbiome[^1]. When this axis is functioning optimally, it promotes a well-balanced immune response. However, dysbiosis, or an imbalance in gut bacteria, can lead to chronic inflammation and diseases.
The Role of the Gut Microbiome in Immunity
Immune Modulation
The gut microbiome plays a key role in modulating the immune response. Specific strains of beneficial bacteria, such as Lactobacillus and Bifidobacterium, promote the production of anti-inflammatory cytokines while inhibiting pro-inflammatory ones[^2]. This helps maintain a balanced immune response, preventing conditions like allergies, autoimmune diseases, and chronic inflammation.
Pathogen Defense
The gut microbiome acts as a barrier against pathogens. Beneficial bacteria compete with harmful microbes for nutrients and attachment sites in the gut lining. Moreover, they produce substances like short-chain fatty acids (SCFAs) that strengthen the intestinal barrier and enhance the production of mucus, which further protects against pathogens[^3].
Education of Immune Cells
The gut microbiome is instrumental in the development of immune cells. For example, dendritic cells in the gut can sample the microbiome, educating T cells to recognize and respond appropriately to pathogens[^4]. This education process is vital for establishing immune tolerance, preventing allergic responses, and ensuring a robust defense against infections.
Factors Affecting Gut Health
Diet
Diet is a significant factor affecting the gut microbiome composition and, consequently, immune function. Diets rich in fiber, fruits, and vegetables promote the growth of beneficial bacteria. On the other hand, high sugar and high-fat diets can lead to dysbiosis, elevating inflammation levels and compromising immunity[^5].
Stress
Chronic stress can negatively affect gut health by altering gut permeability and microbiome composition. It can lead to the release of stress hormones like cortisol, which may inhibit immune function and promote inflammation[^6]. Finding ways to manage stress through techniques such as mindfulness or exercise can have profound effects on both gut health and immune vitality.
Lifestyle Factors
Lifestyle choices such as physical activity, sleep, and smoking can also influence gut and immune health. Regular exercise enhances gut health by promoting microbial diversity, and adequate sleep strengthens the immune response. On the contrary, smoking is linked to alterations in the gut microbiome and has a detrimental effect on overall health[^7].
The Impact of Gut Health on Diseases
Autoimmune Disorders
Autoimmune disorders occur when the immune system mistakenly attacks healthy cells in the body. Research has shown that gut dysbiosis can lead to increased intestinal permeability, allowing bacteria and toxins to enter the bloodstream and trigger autoimmune responses. Conditions like rheumatoid arthritis, multiple sclerosis, and inflammatory bowel diseases (IBD) have been linked to gut health[^8].
Allergies
Gut health is also implicated in the development of allergies. A diverse microbiome, particularly in early life, helps to train the immune system to recognize allergens without overreacting. Dysbiosis during infancy has been associated with a higher incidence of allergies and asthma later in life[^9].
Infections
A healthy gut microbiome plays a vital role in protecting against infections. The balance of microorganisms can dictate how well the body responds to various pathogens. For instance, certain probiotic strains have been shown to reduce the duration and severity of respiratory infections[^10].
Enhancing Gut Health for Better Immunity
Probiotics and Prebiotics
Probiotics are live microorganisms that provide health benefits when consumed in adequate amounts. They can help improve the composition of the gut microbiome and enhance immune function. Common probiotic strains include Lactobacillus and Bifidobacterium, found in yogurts and fermented foods.
Prebiotics, on the other hand, are non-digestible fibers that feed beneficial gut bacteria. Foods high in prebiotics include garlic, onions, asparagus, and bananas[^11]. Incorporating both probiotics and prebiotics in your diet can help maintain a balanced gut microbiome and support immune health.
Dietary Adjustments
A diet rich in whole foods, particularly fruits, vegetables, whole grains, and healthy fats, is essential for promoting gut health. Foods high in fiber not only nourish beneficial bacteria but also promote regular bowel movements, helping to eliminate toxins[^12]. Conversely, reducing the intake of processed foods, sugars, and unhealthy fats can reduce inflammation and improve gut health.
Lifestyle Changes
Incorporating regular physical activity is vital for maintaining a healthy gut. Exercise has been shown to promote microbial diversity and enhance immune function. Additionally, prioritizing sleep is crucial, as poor sleep is linked to a weakened immune response[^13]. Stress management techniques, such as yoga and meditation, can also be beneficial.
Conclusion
The gut-immune connection is a crucial aspect of overall health that cannot be overlooked. By maintaining a healthy gut, we not only improve our digestive function but also enhance our immune response, reducing the risk of various diseases. With simple dietary and lifestyle changes, we can take significant strides toward better gut health and, consequently, a stronger immune system.
As ongoing research continues to unravel the complexities of the gut-immune connection, it is clear that nurturing our gut health is essential for well-being. Whether through adopting a balanced diet, incorporating probiotics, managing stress, or ensuring adequate sleep, we all have the power to improve our gut health and fortify our immune systems. Prioritizing this connection can lead to a healthier, more resilient life.
Footnotes
[^1]: Da Silva, J. S., et al. (2020). "Gut Microbiota and Immune Function: The Role of Microbial Metabolites." Journal of Immunology Research. [^2]: Ramanan, D., et al. (2021). "Role of Gut Microbiota in Modulating Immunity." Clinical Reviews in Allergy & Immunology. [^3]: Louis, P., & Flint, H. J. (2017). "Formation of Short-Chain Fatty Acids by the Gut Microbiota." Nature Reviews Microbiology. [^4]: Ganal-Vonarburg, S. C., et al. (2020). "The Role of the Gut Microbiome in Immunity." Nature Reviews Immunology. [^5]: Tilg, H., & Moschen, A. R. (2014). "Microbiota and metabolic disease." Journal of Clinical Endocrinology & Metabolism. [^6]: Farahani, M. N., et al. (2019). "Impact of Stress on the Gut Microbiome." Frontiers in Microbiology. [^7]: Zhao, L. (2013). "The gut microbiome and obesity: a host-microbiome interaction." Nature Reviews Endocrinology. [^8]: Elinav, E., et al. (2016). "Infectious Disease: The gut microbiome and autoimmunity." Nature Reviews Immunology. [^9]: Voreades, N., et al. (2014). "The Human Microbiome in Health and Disease." The Frontiers in Microbiology. [^10]: Hempel, S., et al. (2012). "Probiotics for the prevention and treatment of antibiotic-associated diarrhea." Cochrane Database of Systematic Reviews. [^11]: Slavin, J. (2013). "Fiber and prebiotics: mechanisms and health benefits." Nutrients. [^12]: Reimer, R. A., et al. (2019). "Dietary strategies to regulate gut microbiota." Gut Microbes. [^13]: Besedovsky, L., & del Rey, A. (2019). "Cytokines and the Immune System: The Role of Sleep." Biological Psychology.




















Add Comment