Bracing for Impact: How Our Skeletons Adapt to Stress and Injury
Introduction
The human skeleton is often seen merely as a framework for our bodies, a rigid structure that supports us in our daily activities. However, it is much more than that; it is a dynamic, living system that adapts and responds to the stresses and injuries it encounters throughout our lives. This article delves deep into the fascinating world of skeletal adaptation, exploring how bones respond to physical stress, the processes of healing after injuries, and the implications for overall health and fitness.
In recent years, research in the fields of biomechanics, physiology, and orthopedics has shed light on how our skeletons cope with the challenges posed by gravity, impact, and injury. This adaptive capability is not only vital for athletes and active individuals but is also crucial for aging populations and those recovering from trauma. Through understanding these mechanisms, we can harness knowledge for better injury prevention and treatment strategies.
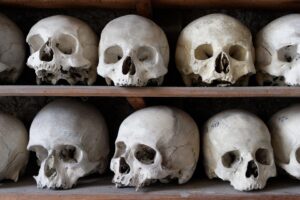
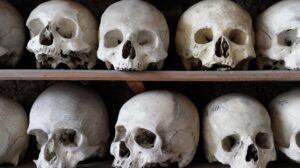
The Anatomy of the Skeleton
Overview of Bone Structure
The human skeleton is composed of 206 bones in adults, each exhibiting a unique structure and function. It can be divided into two main categories:
-
Axial Skeleton: Comprising the skull, vertebral column, and rib cage, the axial skeleton provides stability and protection for vital organs.
- Appendicular Skeleton: Comprising the bones of the limbs and girdles, the appendicular skeleton facilitates movement and interaction with the environment.
Bone tissue itself consists of two main types:
- Cortical Bone: The dense outer layer that provides strength.
- Trabecular Bone: The spongy inner layer that absorbs shock and reduces weight.
Cellular Composition of Bone
Bones are dynamic organs composed of several different types of cells, including:
- Osteoblasts: Cells responsible for bone formation.
- Osteoclasts: Cells that reabsorb bone tissue.
- Osteocytes: Mature bone cells that maintain the bone matrix.
These cells cooperate in a continuous cycle of remodeling, responding to mechanical stress and injury, allowing bones to adapt their density, strength, and shape.
The Science of Bone Adaptation
Mechanotransduction: How Bones Sense Stress
The process by which bones sense mechanical stress is known as mechanotransduction. When bones are subjected to load, they experience minute deformations, which stimulate the bone cells to respond. Research has shown that this response largely depends on a combination of biochemical signaling pathways and physical stimuli.
-
Mechanical Loading: Activities such as weightlifting, running, and jumping apply load to the skeleton, prompting an increase in bone mass and density.
-
Fluid Flow: When bones are loaded, the interstitial fluid within them flows, causing shear stress on the bone surface, which further stimulates osteocytes to signal bone remodeling.
- Hormonal Influence: Hormones like parathyroid hormone (PTH) and calcitonin play significant roles in regulating bone remodeling in response to mechanical stress.
The Role of Wolff’s Law
Wolff’s Law states that bone adapts to the loads under which it is placed. This principle suggests that:
- Increased mechanical stress leads to increased bone density and strength.
- Decreased mechanical stress leads to bone resorption and weakened structure.
This is evidenced in athletes whose skeletal structures adapt to their specific sports and activities. For example, a runner may develop denser tibial bones compared to a sedentary individual due to the consistent impact of running.
Injury and Bone Healing
Types of Bone Injuries
Bone injuries can occur due to various factors, including trauma, repetitive stress, or pathological conditions. Common types of bone injuries include:
- Fractures: Breaks in the continuity of the bone due to excessive force.
- Stress Fractures: Tiny cracks in the bone caused by repetitive strain over time.
- Osteoporosis: A condition where decreased bone density leads to increased fracture risk.
The Healing Process
Bone healing is a complex, multi-phase process that can generally be divided into four stages:
-
Hematoma Formation: Immediately following a fracture, blood collects at the injury site, forming a hematoma that provides a scaffold for incoming cells.
-
Fibrocartilaginous Callus Formation: Granulation tissue forms, and cells differentiate into chondroblasts, creating a fibrocartilaginous callus that bridges the fracture gap.
-
Bony Callus Formation: Osteoblasts replace the fibrocartilage with bony tissue, forming a hard callus.
- Bone Remodeling: The final stage involves remodeling of the bone to restore its original structure, which can take several months to years.
Factors Influencing Bone Healing
Various factors can influence the rate and effectiveness of bone healing, including:
- Age: Younger individuals generally heal faster than older adults.
- Nutrition: Adequate intake of calcium, vitamin D, and protein is crucial for bone regeneration.
- Activity Level: Controlled physical activity can stimulate healing, while excessive immobilization can delay recovery.
Implications for Health and Fitness
The Importance of Bone Health
Understanding skeletal adaptation underscores the importance of maintaining bone health throughout life. Strategies to improve bone health include:
-
Weight-Bearing Exercises: Activities that require support of body weight stimulate bone remodeling and increase bone density.
-
Proper Nutrition: A diet rich in calcium and vitamin D is essential for optimal bone health.
- Preventing Falls: Especially in older adults, fall prevention strategies are vital to reduce the risk of fractures.
Bone Health in Athletic Training
Athletes must be aware of the delicate balance between training and overtraining. While proper training can lead to improved bone density and strength, excessive or unbalanced training may cause stress fractures or long-term damage. Strategies include:
- Cross-Training: Incorporating a variety of activities to prevent overuse injuries.
- Recovery Time: Allowing time for rest and recovery to let bones heal and remodel.
Aging and Bone Health
As we age, maintaining bone health becomes increasingly important due to the risk of osteoporosis and fractures. Strategies for older adults include:
- Regular Exercise: Engaging in weight-bearing and strength-training exercises to promote bone density.
- Nutrition: Ensuring adequate intake of essential nutrients to support bone metabolism.
Future Research Directions
Advanced Imaging Techniques
Recent advances in imaging technologies offer new possibilities for studying bone adaptation and healing. Techniques such as:
- DXA (Dual-Energy X-ray Absorptiometry) provide detailed insights into bone density changes over time.
- MRI and CT Scans allow for non-invasive monitoring of soft tissues around bones.
Genetic Factors in Bone Adaptation
Ongoing research is exploring the genetic underpinnings of bone density and strength. Understanding how specific genes influence bone remodeling can lead to novel interventions for those at risk for injuries or conditions such as osteoporosis.
Biomechanics and Virtual Reality
The use of virtual reality in assessing movements can improve our understanding of how mechanical loading affects bone adaptation. By simulating different activities, researchers can study how variations in technique influence stress on bones.
Conclusion
The human skeleton is an incredible organ system capable of adapting to the stresses and strains of life. From the process of mechanotransduction to the complex healing mechanisms after injury, our bones exhibit a remarkable ability to respond to and recover from various challenges. By understanding these principles, we can take proactive measures to enhance our bone health, reduce the risk of injuries, and improve our overall quality of life.
References
[1] Wolff, J. "Ueber Das Gesetz Der Transformation Der Knochen." Archived; 1892.[2] Frost, H. "The Mechanostat: A Proposed Mechanical System to Explain Bone Remodeling." Bone, 1987.
[3] Raisz, L. "Bone and Mineral Metabolism." The New England Journal of Medicine, 2005.
[4] Harrison, B. "Understanding Bone Healing: A Review." Clinical Orthopedics and Related Research, 2010.
[5] Khan, K. "Stress Fractures: Pathophysiology and Treatment." Sports Medicine, 2012.
[6] NIH Osteoporosis and Related Bone Diseases National Resource Center. "Bone Health and Osteoporosis: A Report of the Surgeon General." U.S. Department of Health and Human Services, 2004.
[7] Maddalozzo, G. "Physical Activity and Bone Health in Older Adults." Journal of Bone and Mineral Research, 2010.
[8] Jiang, Y. "The Role of Nutrition in Maintaining Bone Health." Nutrition Reviews, 2015.
This article serves as an overview of how our skeletons adapt to stress and injury, summarizing the fundamental concepts and latest research findings in this area. Further exploration into this topic can provide deeper insights into preventive care, rehabilitative strategies, and the future of bone health management.






















Add Comment