The Aging Bones: Understanding Osteoporosis and Its Impact
Introduction
Osteoporosis is often termed a "silent disease," as it typically progresses without obvious symptoms until a fracture occurs. It is characterized by a decrease in bone density, leading to fragile bones that are more susceptible to fractures. As the world’s population ages, understanding osteoporosis becomes increasingly crucial. This article will explore the nature of osteoporosis, risk factors, prevention strategies, and its societal impact, utilizing reliable modern sources throughout.
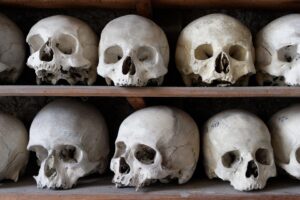
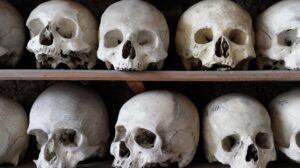
What is Osteoporosis?
Osteoporosis is a condition that results in decreased bone density, making bones thinner, weaker, and more prone to fractures. The World Health Organization (WHO) defines osteoporosis as a bone mineral density (BMD) that is 2.5 standard deviations or more below the average healthy peak bone mass. This condition primarily affects older adults, especially postmenopausal women, but can also occur in men and younger populations due to various factors.
Bone Remodeling
To understand osteoporosis, it is essential to grasp the concept of bone remodeling. The human skeleton is dynamic and undergoes constant remodeling through two primary processes: bone resorption and bone formation. Osteoclasts break down old bone, while osteoblasts create new bone. In osteoporosis, resorption outpaces formation, leading to a net loss of bone density over time[^1].
Risk Factors
Several risk factors contribute to the development of osteoporosis, categorized into modifiable and non-modifiable factors.
-
Non-modifiable Risk Factors:
- Age: Bone mass peaks around 30 years and declines with age.
- Gender: Women are at greater risk, especially post-menopause due to decreased estrogen levels.
- Family History: A family history of osteoporosis increases risk.
- Ethnicity: Caucasian and Asian descent have higher risks compared to African descent.
- Modifiable Risk Factors:
- Diet: Insufficient intake of calcium and vitamin D can lead to weakened bones.
- Physical Inactivity: Weight-bearing exercises strengthen bones.
- Smoking: Tobacco use is linked to lower bone density.
- Alcohol Consumption: Excessive alcohol can interfere with calcium absorption.
Symptoms and Diagnosis
Osteoporosis is often asymptomatic in its early stages. Many individuals do not realize they have the disease until they experience a fracture. Common types of fractures associated with osteoporosis occur in the hip, spine, and wrist[^2].
Diagnosis typically involves:
- Bone Density Testing: Dual-energy X-ray absorptiometry (DEXA) scans measure BMD.
- Blood Tests: These may assess calcium levels, vitamin D, and other hormones that influence bone health.
The Impact of Osteoporosis
Osteoporosis has far-reaching implications, not only for the individual but also for public health systems.
Personal Impact
-
Fractures and Mortality: Osteoporotic fractures lead to significant morbidity and mortality. Studies suggest that individuals over the age of 50 may experience an increased risk of death following hip fractures[^3].
-
Quality of Life: Fractures can severely impact mobility and independence, leading to physical limitations and psychological issues, including depression. The fear of falling can restrict activities, further contributing to social isolation[^4].
- Healthcare Costs: Osteoporosis-related fractures contribute substantially to healthcare costs, including hospitalizations, long-term care, and rehabilitation services[^5].
Societal Impact
-
Economic Burden: In the United States, the estimated direct healthcare costs related to osteoporosis were around $19 billion in 2018[^6]. As the population ages, these costs are expected to rise significantly.
-
Workforce Implications: Osteoporosis may impact workforce participation, particularly if older individuals are unable to continue in their roles due to health issues.
- Public Health Policies: Governments may need to address osteoporosis through strategies that include health education, screening programs, and initiatives promoting active lifestyles among the elderly[^7].
Prevention Strategies
Nutrition
-
Calcium Intake: It is essential to meet the recommended dietary allowance (RDA) for calcium, which varies by age and sex. Good sources include dairy products, leafy greens, and fortified foods.
- Vitamin D: This vitamin plays a crucial role in calcium absorption. Sun exposure, supplementation, and dietary sources such as fatty fish can help maintain adequate levels.
Physical Activity
Engaging in regular weight-bearing and resistance exercises can strengthen bones and improve balance, significantly reducing the risk of falls[^8]. Recommended activities include:
- Walking
- Dancing
- Weight training
- Tai Chi
Lifestyle Modifications
-
Smoking Cessation: Quitting smoking is vital for bone health.
-
Moderate Alcohol Consumption: Limiting alcohol intake can positively impact bone health.
- Fall Prevention: Implementing safety measures at home, such as removing trip hazards and using assistive devices, can reduce fall risk[^9].
Medical Interventions
For those at high risk or diagnosed with osteoporosis, medical treatment may be necessary. Options include:
- Bisphosphonates: These drugs help slow down bone loss.
- Hormone Replacement Therapy (HRT): In certain scenarios, HRT is recommended for postmenopausal women to maintain bone density.
- Other Medications: New treatments, including monoclonal antibodies and anabolic agents, are being developed and show promise in enhancing bone density[^10].
Conclusion
Understanding osteoporosis is essential as the global population ages. By recognizing risk factors, diagnosing the disease, and implementing prevention strategies, individuals can significantly reduce their risk of osteoporosis-related fractures. Societally, addressing this issue can alleviate economic burdens and enhance the quality of life for the aging population.
Continued education and research into osteoporosis will play a vital role in promoting bone health as we age, ensuring that individuals enjoy active and fulfilling lives.
References
[^1]: National Institutes of Health. (2021). Understanding Osteoporosis.[^2]: World Health Organization. (2018). Osteoporosis: A Brief Guide for Patients.
[^3]: Center for Disease Control and Prevention. (2020). Osteoporosis – Causes and Symptoms.
[^4]: American Bone Health. (2019). Living with Osteoporosis: A Guide.
[^5]: National Osteoporosis Foundation. (2017). Bone Health and Osteoporosis: A Report.
[^6]: Burge, R., et al. (2020). Incidence and Economic Burden of Osteoporosis Fractures in the United States.
[^7]: International Osteoporosis Foundation. (2022). The Global Burden of Osteoporosis.
[^8]: Lee, T. C., et al. (2019). Benefits of Exercise on Bone Health.
[^9]: Geller, E. S. (2018). Fall Prevention in Seniors: Strategies and Solutions.
[^10]: American Society for Bone and Mineral Research. (2021). Advances in Osteoporosis Treatment.






















Add Comment